BECAUSE POSTPARTUM MATTERS
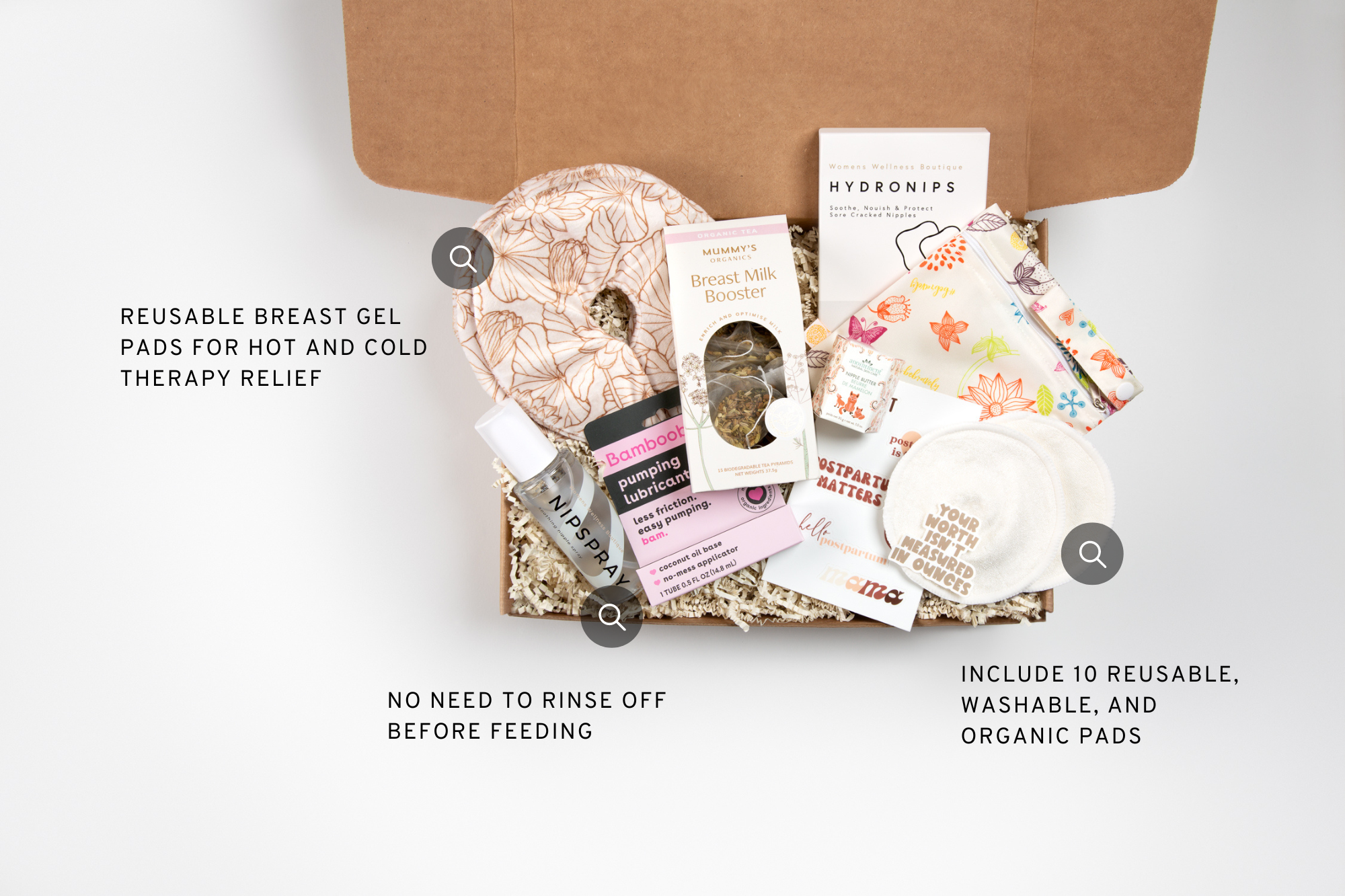
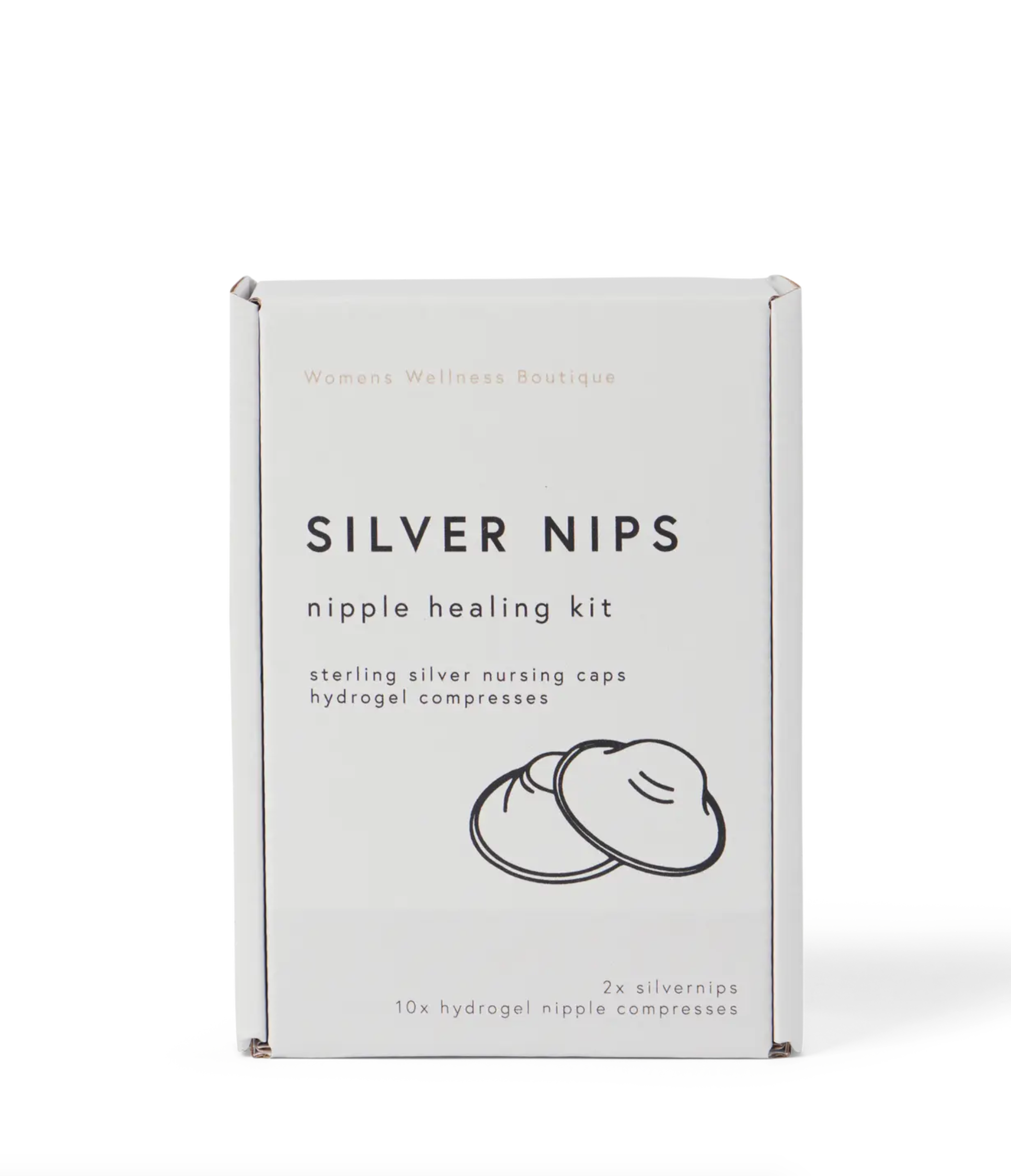
New Mom Gifts & Recovery Essentials, Delivered
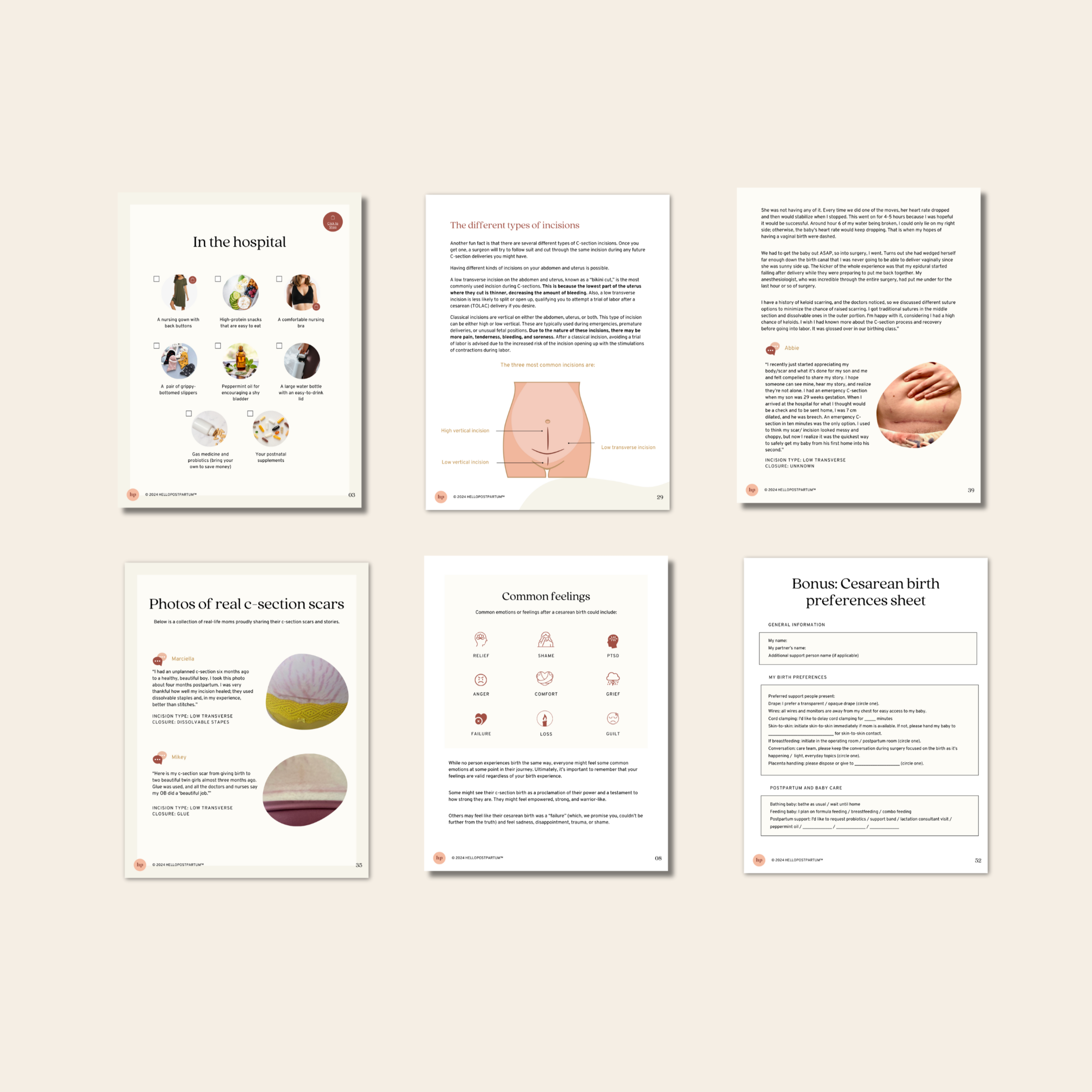
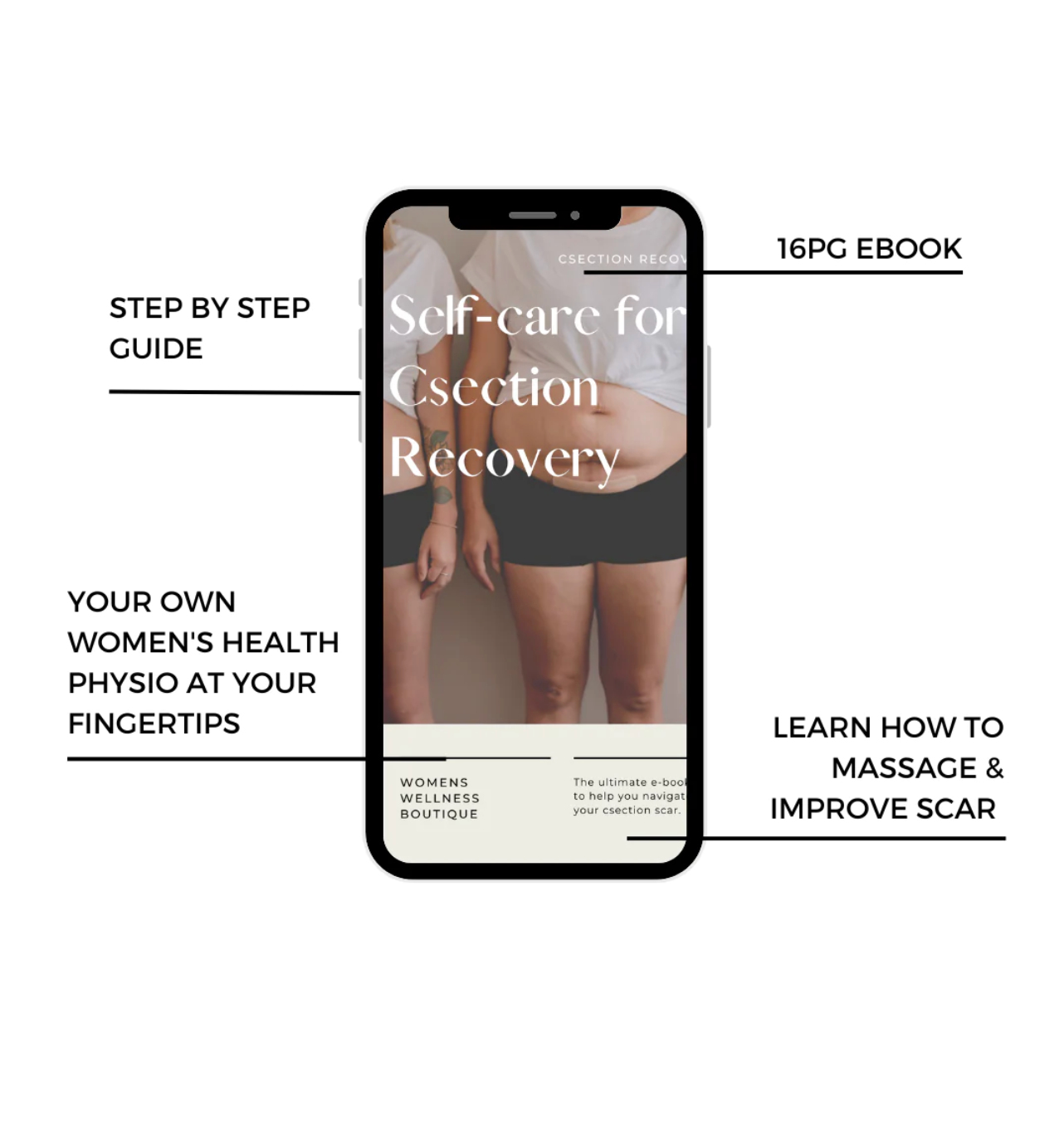
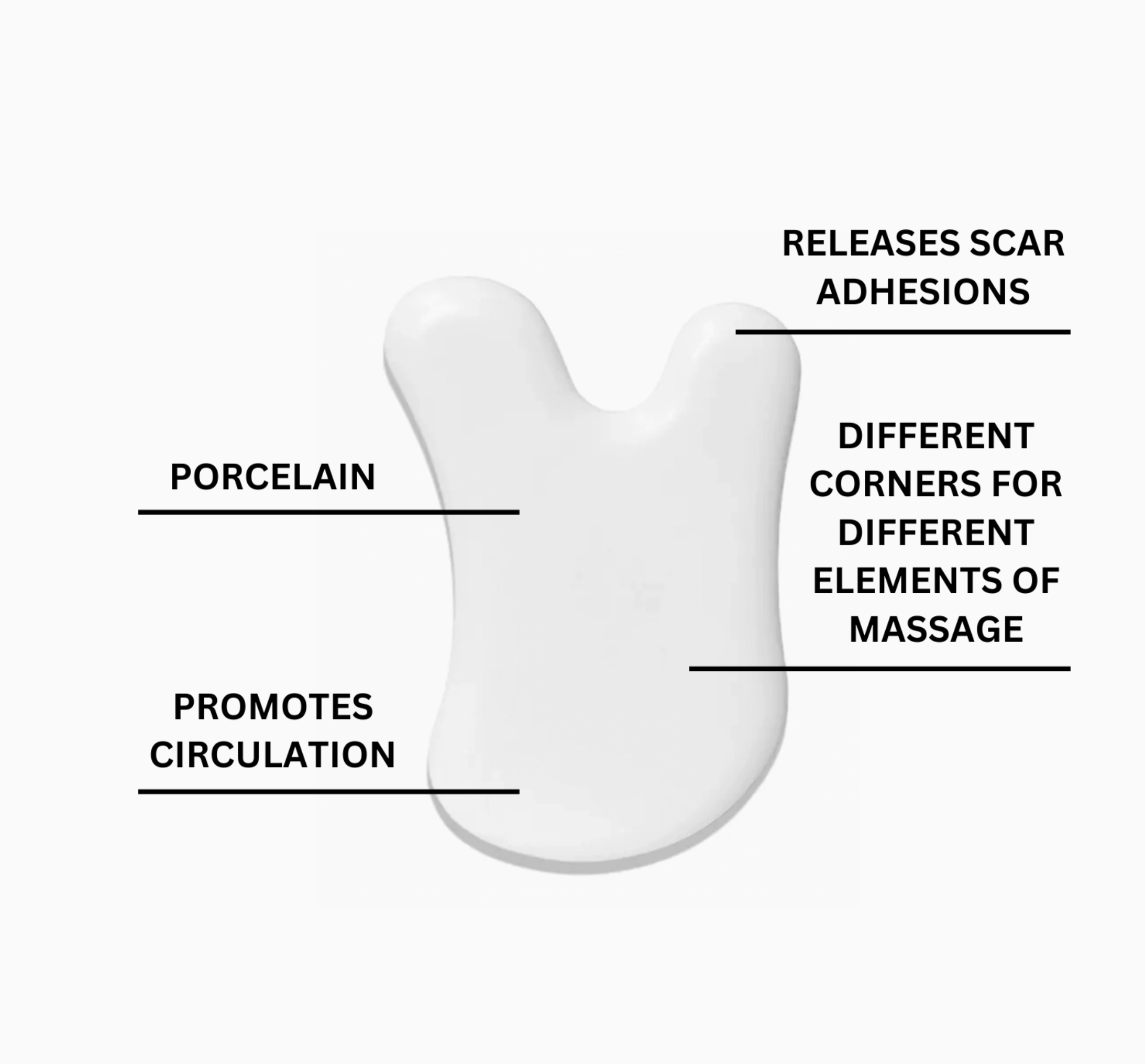
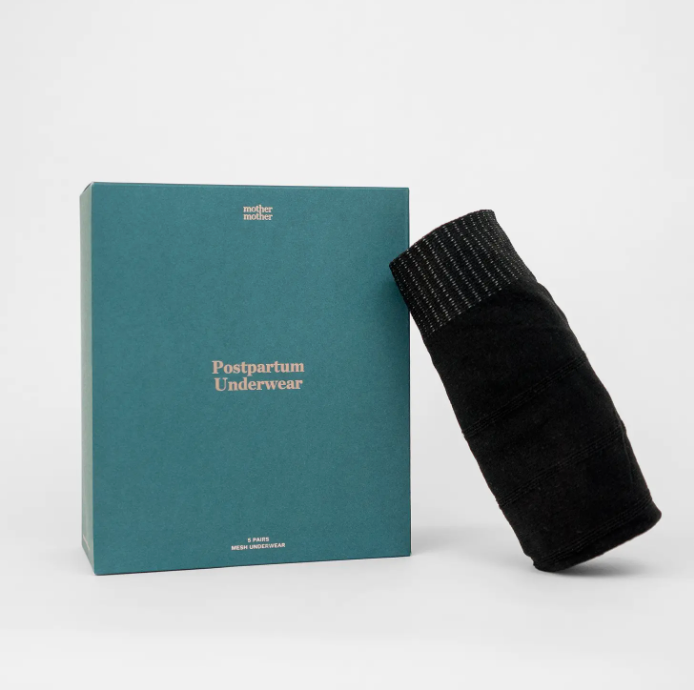
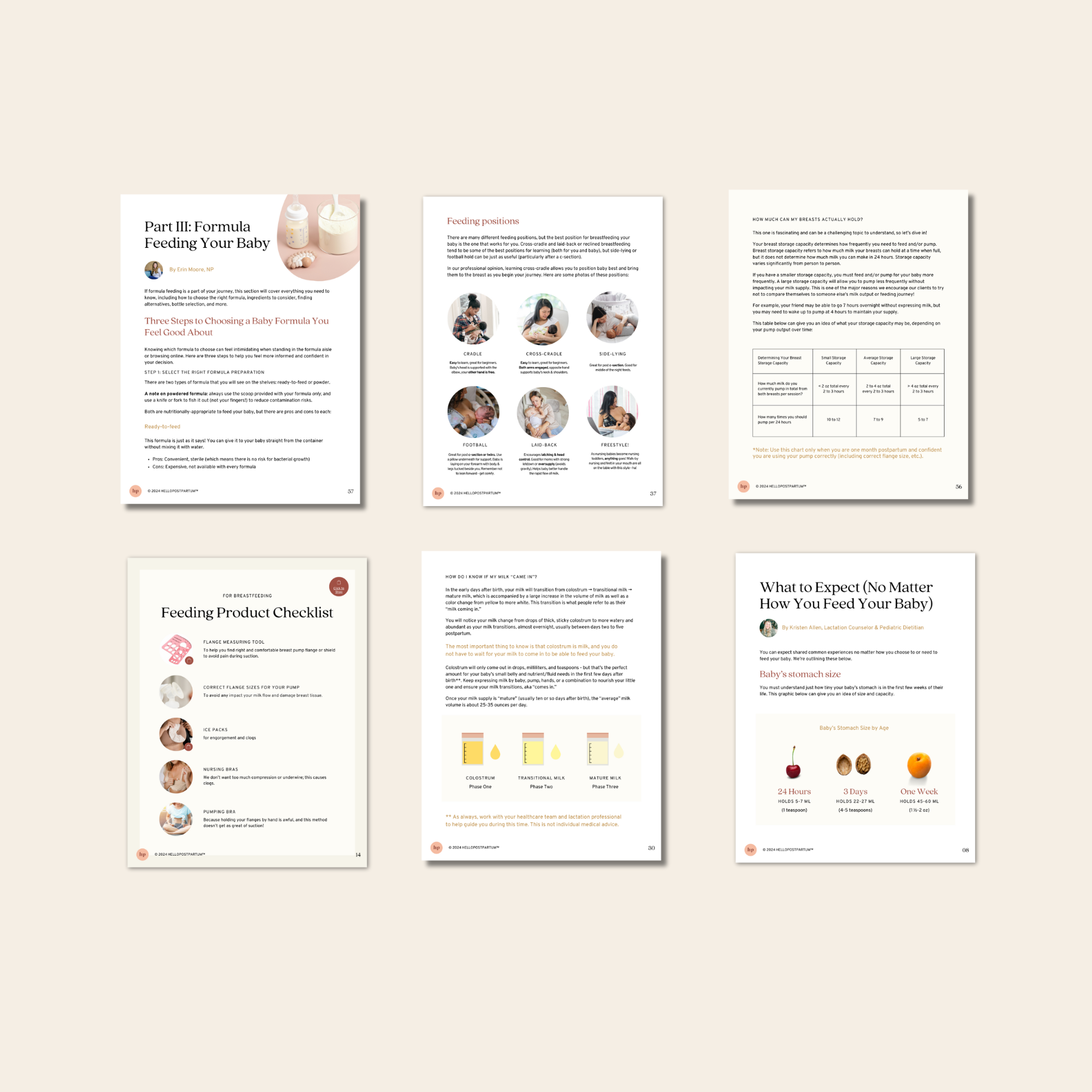
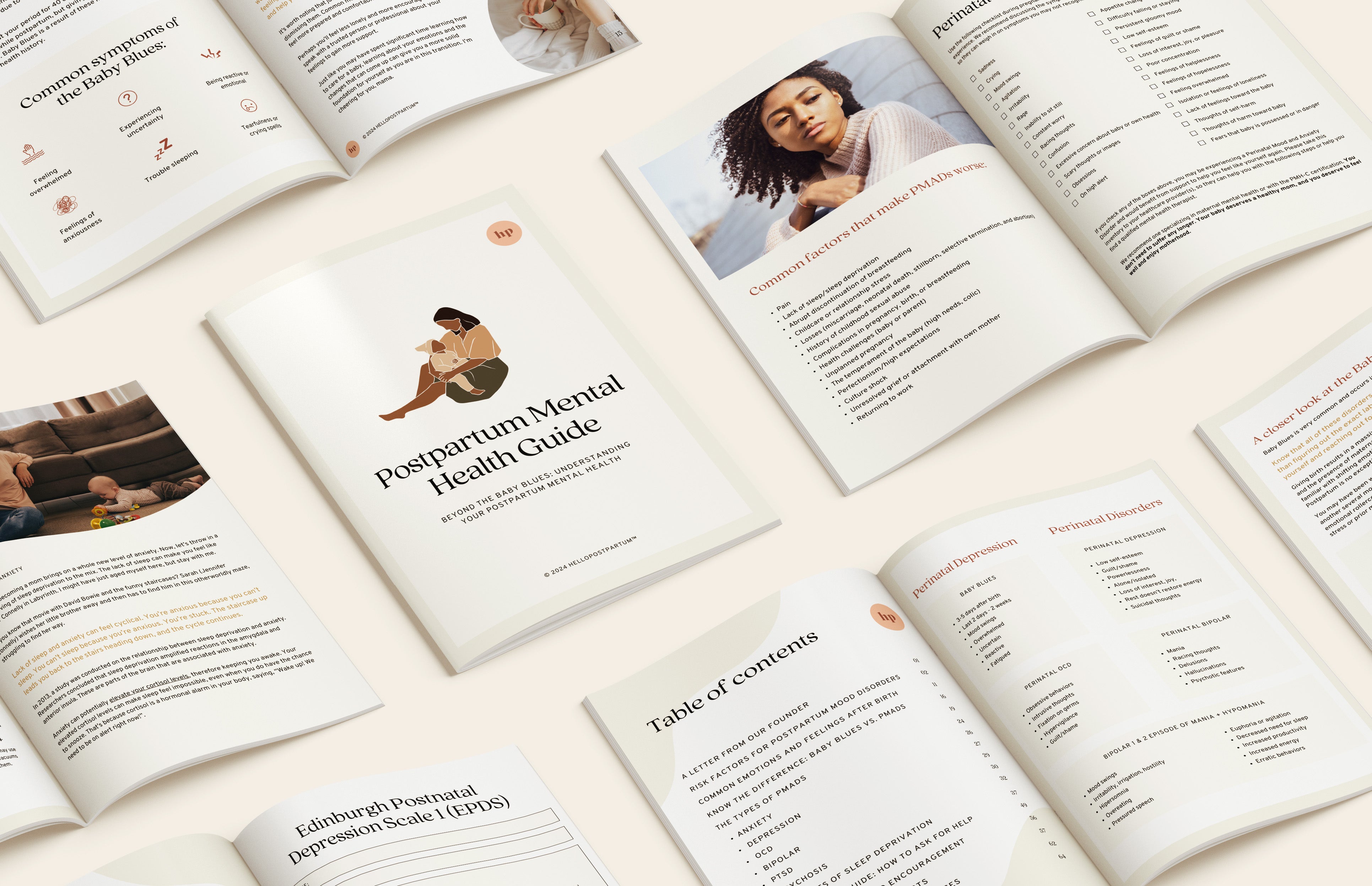
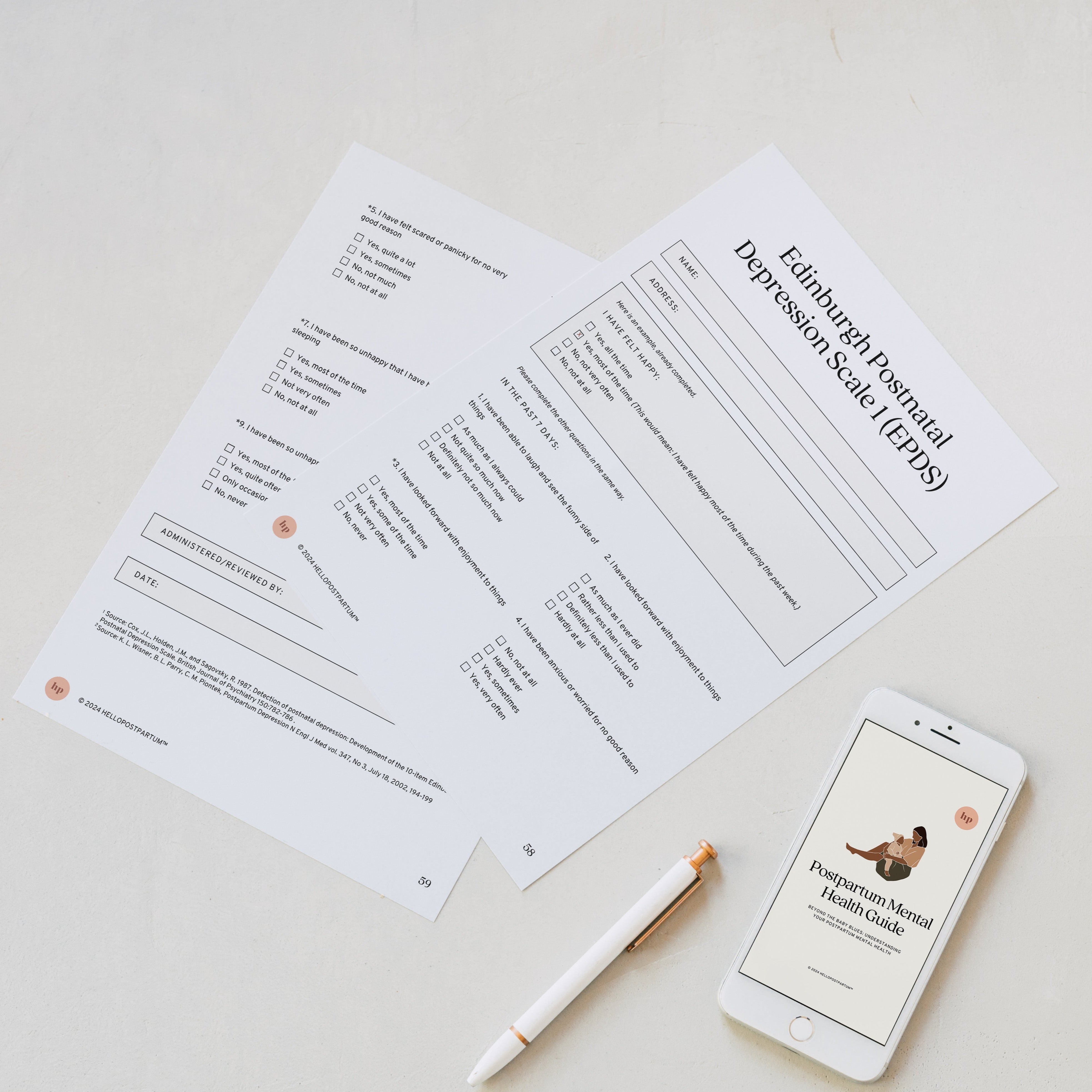
Discover postpartum recovery must-haves, curated or custom gift boxes, and expert-written eBooks, all designed to support life after birth.

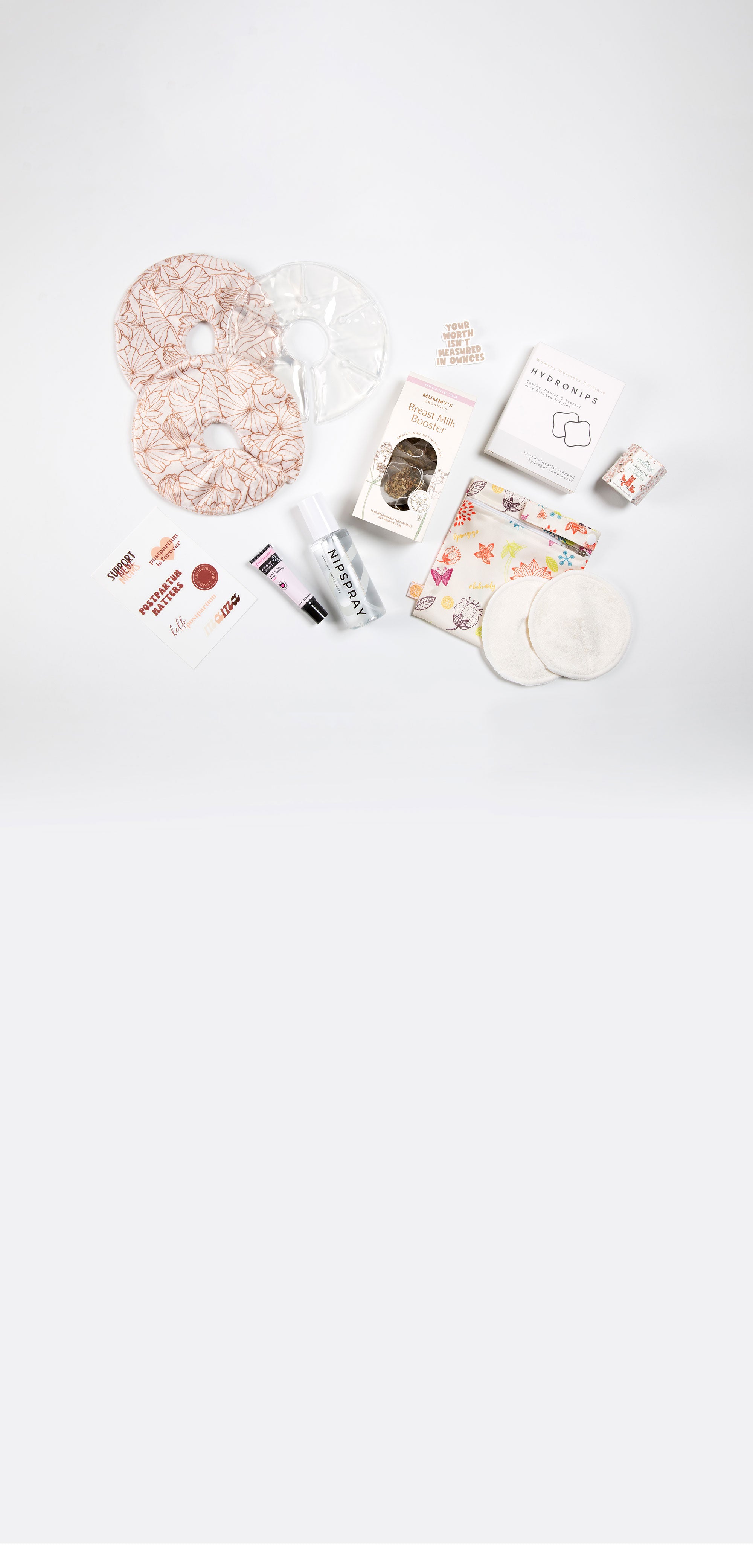
Featured Collections
Build a Postpartum Gift Box
Select your items, we'll handle the rest.

founded in 2020
About Hello Postpartum
We empower new moms through expert-created postpartum eBooks, recovery essentials, and supportive gifts. Baby doesn't need another swaddle, let's support life after birth for every new mom; one box at a time.


Carefully curated