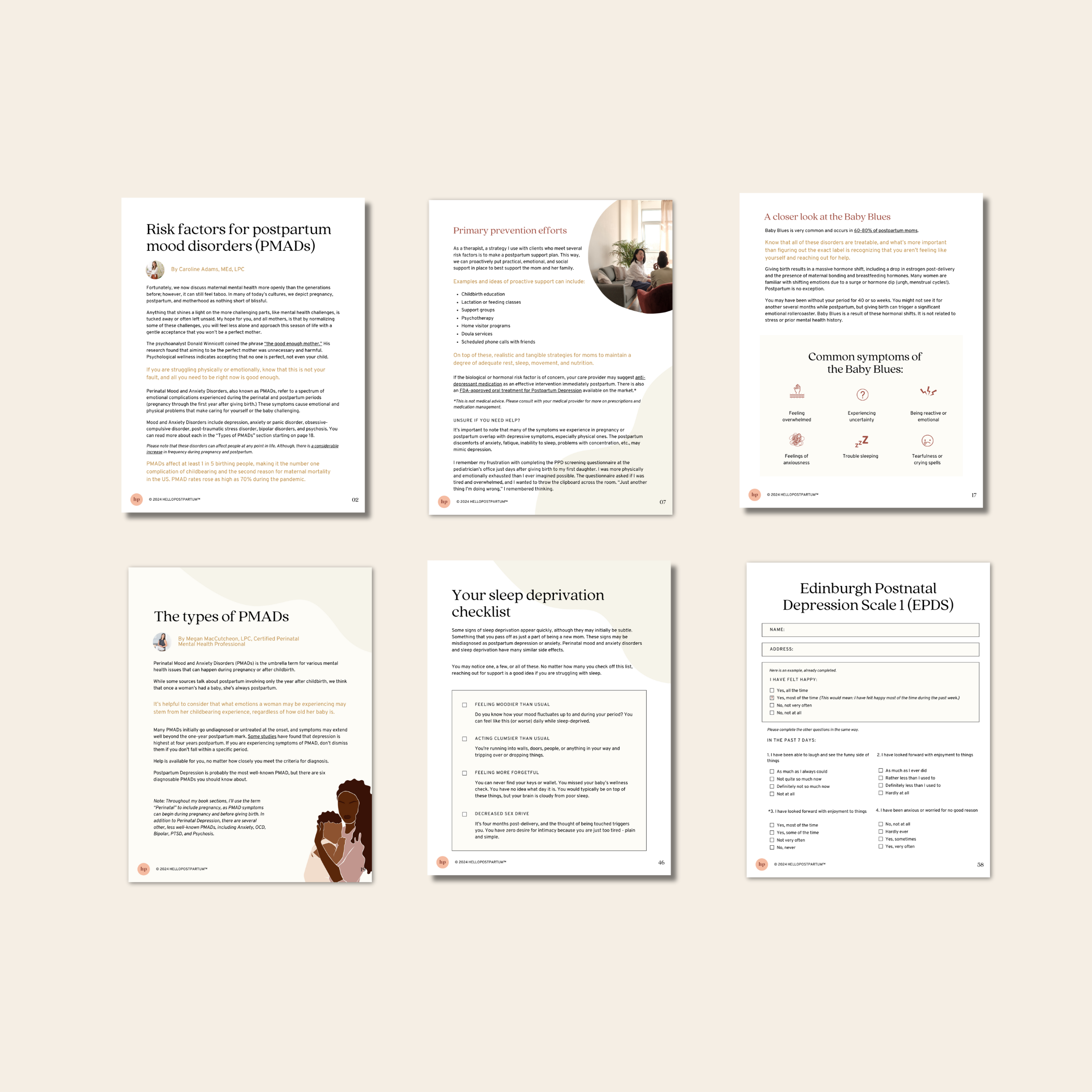
I’m really glad I stumbled upon this resource. My husband and I have friends that were really blindsided by unexpected postpartum mental health issues that resulted in the breakup of their marriage (they had issues to start with, though). They had no plan prior to both able how they would handle mental health issues as a team. We want to try our best to avoid that possibility, so we wanted to learn about what could happen and try to prevent it and then create a plan for what we agree ahead of time we should do if it does happen. We now know what the different issues are that can occur, how common they are, how to spot them, and how they differ from baby blues. We used this guide plus the free postpartum planning guide to know how to create a prevention plan. I printed out the checklist for us to just hang on the fridge so that we can see if I’m (or he is) meeting any of the criteria, and we are in the process of identifying a postpartum therapist that we can call on if needed in postpartum (plus we will try to see them once before birth to go over our plan with them and get their input). My husband and I have never had mental health issues before so I had no idea where to start in planning for preventing or coping with a postpartum mental health issue and after reading this I feel completely confident and prepared! As a health professional myself (Registered Dietitian) I also love that it was written by qualified health professionals and wouldn’t have purchased it otherwise!